Understanding the Risk of Cervical Cancer After Hysterectomy
Hysterectomy, a surgical procedure that involves the removal of the uterus, is often performed for various medical reasons such as fibroids, endometriosis, or cancer. While this procedure can significantly improve a woman's quality of life, it's essential to consider its implications, particularly concerning the risk of cervical cancer after hysterectomy. This article will delve deeply into this subject, analyzing the factors at play and providing you with critical information for informed health decisions.
What is Hysterectomy?
A hysterectomy can be classified into several types, depending on how much of the uterus and surrounding structures are removed:
- Total Hysterectomy: Removal of the entire uterus and cervix.
- Partial or Subtotal Hysterectomy: Removal of the upper part of the uterus, leaving the cervix intact.
- Radical Hysterectomy: Removal of the uterus, cervix, part of the vagina, and surrounding tissue, typically done for cancer treatment.
Understanding the type of hysterectomy performed is crucial in assessing the risk of cervical cancer after hysterectomy.
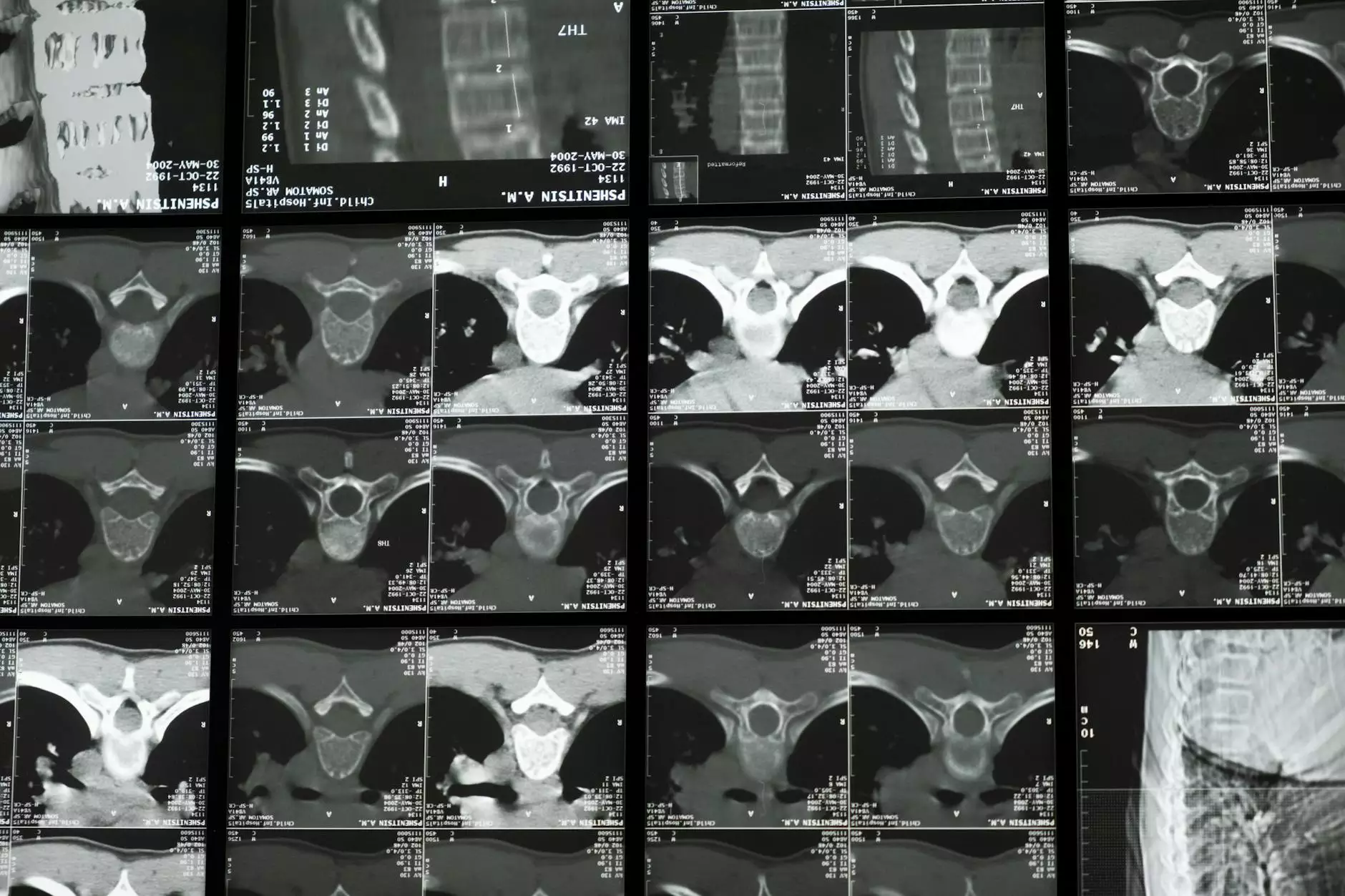
The Cervix and Its Role in Women's Health
The cervix serves as the lower part of the uterus and plays a vital role in a woman's reproductive system. It produces mucus that changes in consistency during the menstrual cycle and acts as a barrier to bacteria and other pathogens. Cervical health is often monitored through regular Pap smears, which can detect early signs of cervical cancer or precancerous conditions.
Effect of Hysterectomy on Cervical Cancer Risk
One common misconception is that having a hysterectomy eliminates the risk of cervical cancer entirely. However, this is not entirely accurate. The risk of cervical cancer after hysterectomy is influenced by several factors:
1. Type of Hysterectomy
The type of hysterectomy performed can have varying implications on cervical cancer risk. In total hysterectomies, where both the uterus and cervix are removed, the risk of cervical cancer is eliminated because the cervix, where most cervical cancers develop, is no longer present. However, if a woman undergoes a subtotal hysterectomy, retaining the cervix, she may still be at risk for developing cervical cancer, especially if she has a history of HPV (Human Papillomavirus) infection.
2. HPV and Cervical Cancer
HPV is a leading cause of cervical cancer. Many women are infected with HPV during their lives, but most clear it without any complications. However, persistent infection with high-risk HPV types can lead to changes in the cervical cells, resulting in cancer. If a woman has a history of HPV prior to her hysterectomy, she may be at an increased risk for cervical cancer if she retains her cervix. It's crucial for such women to maintain regular check-ups and screenings.
3. Underlying Health Conditions
Other health conditions, such as a compromised immune system due to HIV/AIDS or immunosuppressive medications, can also affect the risk of developing cervical cancer post-hysterectomy. Women with such conditions are advised to follow their healthcare provider's recommendations for ongoing screenings and preventive care, even after undergoing a hysterectomy.
Monitoring Cervical Health After Hysterectomy
Importance of Regular Screenings
For women who have undergone a subtotal hysterectomy, it is essential to continue scheduling regular Pap smears and HPV tests as recommended. Regular screenings can aid in the early detection of any abnormal cell changes that could lead to cervical cancer.
Post-Hysterectomy Follow-Up Care
Follow-up care after a hysterectomy is crucial for monitoring overall reproductive health. This can include:
- Regular pelvic exams
- Consultations regarding hormonal health if the ovaries were removed
- Discussions about any ongoing symptoms or concerns
Preventive Measures for Cervical Cancer
To mitigate the risk of cervical cancer after hysterectomy, women, especially those at higher risk, should consider the following preventive strategies:
1. HPV Vaccination
The HPV vaccine is recommended for preteens and can be administered up to age 45. This vaccine protects against the types of HPV that most commonly cause cervical cancer. Vaccination can dramatically reduce the risk of developing cervical cancer later in life.
2. Safe Practices
Engaging in safe sexual practices can reduce the likelihood of HPV transmission. This includes using barriers such as condoms and having regular screenings for sexually transmitted infections.
3. Healthy Lifestyle Choices
Maintaining a healthy lifestyle can support overall reproductive health. This includes:
- A balanced diet rich in fruits, vegetables, and whole grains
- Regular physical activity
- Avoiding tobacco products
- Limiting alcohol consumption
Conclusion
The risk of cervical cancer after hysterectomy is a critical topic for women to understand, particularly those with a history of cervical health issues or HPV infections. While the absolute risk may vary depending on the type of hysterectomy and individual health factors, awareness, and prevention are key to maintaining cervical health.
Regular medical check-ups and adhering to recommended screening protocols can empower women to take control of their health. As always, if you have any concerns or questions related to your health, it is crucial to engage with a knowledgeable healthcare provider.
For more information on women's health and management of cervical health issues, visit Dr. Seckin's website where you can find valuable resources and expert guidance.